Let’s Talk!
Most of us are familiar with condoms. This barrier method of contraception is widely used throughout the world. However, there may still be facts about condoms that you don’t know. I will explore the origins of condoms, the various kinds available, and the role they play in heterosexual relationships.
The origin of the word “condom†appears to be unknown. Condoms are also called prophylactics, rubbers, and in Great Britain, French letters. Some people refer to condoms by the name of the manufacturer: for example, a Trojan.
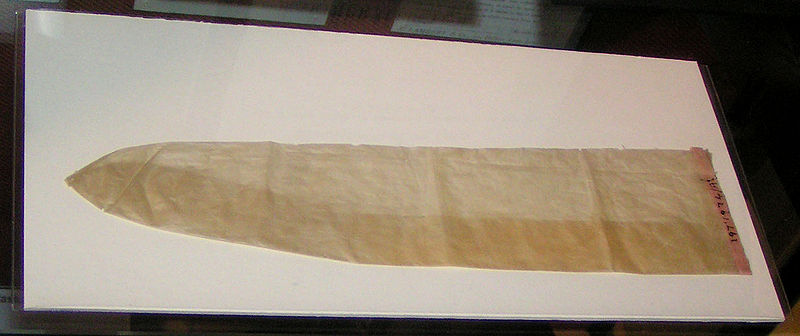
Condoms—in various forms—have been used for the past 400 years. In the 15th century Asia, condoms only covered the tip (or gland) of the penis and were used primarily by the upper class. They were made of oiled silk paper in China and of tortoiseshell or horn in Japan. By the time of the Renaissance in Europe, linen and intestine condoms that covered the whole penis were available.
In the 18th century, most religious, legal and medical authorities opposed the use of condoms because they: 1) could prevent pregnancies; 2) did not protect the user 100% of the time from sexually transmitted infections (STIs); 3) encouraged promiscuity because they provided a false sense of safety; and 4) were not used consistently due to inconvenience, expense, and loss of sensation.
Nevertheless, in 18th century Europe and Russia, condoms were available in a variety of qualities and sizes and were sold in many venues including pubs, barbershops, and open-air markets. However, condoms were used mainly by the upper classes because of the cost and because most members of the lower classes lacked sexual health knowledge.
In 1855, American inventor Charles Goodyear made the first rubber condom. Through the rubber vulcanization process, he was able to make the rubber elastic. These earlier condoms had a seam and were as thick as a bicycle inner tube.
In England and the United States, a smaller version of this kind of rubber condom was often used. This kind only covered the tip (or gland) of the penis. This early type of condom received the French name capote because it resembled a woman’s bonnet worn at that time.
In 1920, latex rubber was invented. Latex condoms were stronger, thinner, and had a shelf life of five years, compared to three months for their rubber counterparts. By 1930, condoms were made in fully automated factories using conveyor systems. This helped drive their price down and turned skin condoms into a niche, high-end market.
The birth control pill was introduced in the 1960s and quickly became the number one birth control method in the world, but condoms were a close second. In the 1970s, tighter quality control regulations for the manufacturing of condoms were implemented, and many laws banning the usage and advertising of condoms were abolished.
The spread of AIDS in the early 1980s helped increase the sale of condoms until the mid-1990s. Although people are now less concerned about contracting AIDS (also called prevention fatigue), it is predicted that worldwide condom use will reach 18.6 billion by 2015.
Today, most condoms are inexpensive, easy to use, cause few side effects, and provide protection against STIs and pregnancy. Male condoms are usually made of latex, but some are also made of polyurethane, polyisoprene, and lamb intestine, while female condoms are fabricated from nitrile.
Modern male condoms for men have a reservoir tip at their end to collect the man’s ejaculate. Condoms come in a variety of sizes—from snug to oversized—and in a variety of textures to help stimulate one’s partner. They also come pre-lubricated to help penetration and flavored for oral sex. The standard male condom has a diameter of 2 inches (4.5 cm) and a length of 7.4 inches (19 cm).
Condoms are usually packaged in a foil wrapper in a rolled-up form and are unrolled over an erect penis. After ejaculation, the best practice is to tie the condom in a knot and dispose of it in a regularly emptied wastebasket.
Modern condoms are made of a variety of materials: natural latex, synthetics (polyurethane & polyisoprene), and lambskin. In addition to condoms for men, a condom for women is also available.
Natural latex condoms have a tensile strength of more than 30 megapascals (MPa) and can be stretched to 8 times their actual length without breaking. Latex can be damaged by oil-based substances such as petroleum jelly, baby oil, mineral oil, and skin lotions. Every latex condom is tested for holes with an electrical current, and a portion of each batch of condoms is subjected to water leakage and air bust testing. Some people are allergic to natural latex because of the protein found in it.
Polyurethane condoms are the most common form of synthetic condoms. They have the same width and thickness as latex condoms, but are better conductors of heat, and are less sensitive to temperature and ultraviolet light. Also, they have a longer shelf life, can be used with oil-based lubricants, are hypoallergenic and do not have an odour. They are as effective as latex condoms in protecting from STIs. However, polyurethane condoms have less tensile strength than latex condoms and tend to slip, break, and bunch up more. Also, they are more expensive.
Polyisoprene condoms are a synthetic type of natural latex condom. They are softer and more elastic than polyurethane condoms and do not cause latex allergies. Also, they are better transmitters of body heat than natural latex, but they cannot be used with oil-based lubricants.
Sheep intestine condoms prevent pregnancies but not STIs, because their pores are big enough for viruses to escape. Sheep intestine condoms are hypoallergenic and some people say that they provide a more “natural†feel. However, these types of condoms tend to be significantly more expensive than latex condoms.
Female condoms have a large stiff ring to keep them from slipping into the vagina. The Female Health Company originally produced polyurethane female condoms, but now they are made of nitrile. A company called Medtech makes latex female condoms.
According to James Trussell Ph.D., Professor of Economics and Public Affairs at Princeton University, when a condom is used perfectly, the pregnancy rate is 2% per year, whereas typical use brings the pregnancy rate up to 15%.
There are a variety of reasons for latex condom failure. The condom
• can slip from the penis after ejaculation,
• break due to improper application (rate between 0.4% and 2.3%),
• be physically damaged during the tearing of the package, or
• degrade or slip if it’s used after the expiry date, improperly stored, or exposed to oils such as Vaseline (rate between 0.6% and 1.3%).
Regardless of these above reasons, about 1-2% of women will have semen residue in their vagina after intercourse with the proper use of a latex condom.
How does the average heterosexual Canadian couple use condoms?
Canadian MD Dhalla Shayesta states that since the early 2000s there has been an increase in reported rates of chlamydia, gonorrhea, and infectious syphilis, while HIV remains a serious sexual health concern.
According to the 2005 Canadian Community Health Survey, sexually active single young adults (30- to 34-year-olds) tend to use condoms less often (54.7%) than their younger (15- to 17-year-old) counterparts (81%). This trend is consistent for both males and females.
The above statistics correlate with the 2010 Public Health Agency of Canada’s report of higher incidence of sexually transmitted infections (STIs) such as chlamydia among the older group of young adults. Since most people have a series of monogamous relationships, over time they expose themselves to many infectious diseases.
There may be a few explanations as to why couples gradually shift away from the use of condoms.
Many young couples may initially use condoms as a method of birth control, not as protection from STIs. Then, as the relationship progresses, they may stop using condoms, perceiving this as a sign that the relationship has taken on a more serious, intimate, and exclusive nature. Only a small proportion of these couples have a serious discussion about sexual health with their partners.
When people consider themselves in a stable monogamous relationship, they tend to turn to other forms of birth control methods (e.g., the birth control pill). Individuals may assume that because their partner does not have any visible signs of an STI, it’s “safe†to have unprotected sex, although most cases of STIs are asymptomatic, and most people do not get tested for STIs.
What complicates matters is that even when couples do decide to get tested for STIs, a general physician usually only tests for HIV and chlamydia as well as performs a PAP test on women to detect changes in the cervix due to a Human Papillomavirus (HPV) infection. People are not routinely tested for two of the most common infections in Canada—genital herpes type two (HSV-2) and HPV.
Different strategies can be used to overcome people’s reticence to continue using condoms.
If couples incorporate putting on a condom into foreplay, they won’t perceive it as a break in the flow of love-making. Also, if they keep in mind that using a condom reduces the risks of STIs, this reassurance can decrease their anxiety, and enhance their relaxation and ability to feel pleasure. Also, intimacy can be cultivated by other means such as shared activities/interests, and exploring other ways of experiencing sexual pleasure (e.g., sensual massages or kissing).
We have come a long way in 400 years—from the capote that only covered the gland to the modern latex condom that covers the whole penis. It took many trials and errors to come up with a design that was low cost and convenient, with the added advantage of protecting the user from pregnancy and most STIs.
With all these advantages, it is intriguing to explore how heterosexual couples use condoms within their relationships. Sexual health is about more than the mechanics of sex: feelings, assumptions, and social/cultural aspects all play a role in how and when people use condoms.
One can only guess what the next generation of condoms will look like. If the present variety of condoms is any indication, we will be pleasantly surprised.
Literary Truths
Here are some interesting facts about condoms:
• Anti-rape condom: Named the Rape-aXe, this condom was invented by Sonnet Ehlers, a South African woman. It is a latex sheath embedded with shafts of sharp, inward-facing barbs and is worn inside the vagina like a female condom. If a man penetrates the woman with his penis, upon withdrawal the penis will be snagged by the barbs, causing the attacker excruciating pain. The Rape-aXe stays attached to the penis and can only be removed surgically at a hospital.
• Collection condoms: These are made of silicone or polyurethane and are used to collect semen for fertility treatments or sperm quality analysis. They are designed to maximize sperm life.
• Boosting condom: This condom has a gel in its tip to help dilate the penis’ arteries, thereby increasing the blood flow and resulting in a firmer and bigger erection.
• Hypoallergenic latex condom: Named Vytex, this is a natural latex condom that has been treated to remove 90% of the protein responsible for latex allergic reactions. A synthetic latex condom (polyisoprene) is also available for people sensitive to natural latex.
• Highest condom usage: According to a Population Reference Bureau 2008 statistic, Japan has the highest condom usage in the world with 80% of Japanese relying on condoms as their birth control method.
• Addition of spermicide: The addition of spermicide (nonoxynol-9) to latex condoms increases the risks of contracting STIs. Nonoxynol-9 irritates the delicate genitalia area, and this increases the risks of tears and the infiltration of bacteria and viruses.
Truth in Motion
References
Bolton, Melissa, Alexander McKay, and Margaret Schneider. “Relational influences on condom use discontinuation: a qualitative study of young adult women in dating relationships.” The Canadian Journal of Human Sexuality 19.3 (2010): 91.
Boyle, Andrea M., and Lucia F. O’Sullivan. “General and sexual communication in established relationships: an exploration of possible links to condom use among young adults.” The Canadian Journal of Human Sexuality 19.1-2 (2010): 53.
Dhalla, Shayesta, and Gary Poole. “Determinants of condom use: Results of the Canadian community health survey 3.1.” Canadian Journal of Public Health 100.4 (2009): 299.
McKay, Alexander, and Michelle Rotermann. “Condom use at last sexual intercourse among unmarried, not living common-law 20- to 34-year-old Canadian young adults.” The Canadian Journal of Human Sexuality 18.3 (2009): 75.
“Why do many older teens and young adults at risk for sexually transmitted infections stop using condoms?” The Canadian Journal of Human Sexuality 20.3 (2011): 119.



STD Testing is something I recommend to all of my friends. I feel it is very important to stay safe and be aware!
I love this site!